Discover the causes of frozen shoulder and how osteopathy can help prevent it—ideal advice for diabetics, post-surgery patients and those leading inactive lifestyles.

Frozen shoulder, or adhesive capsulitis, is a common yet often misunderstood condition characterised by pain and significant restriction of shoulder movement. For many, the prospect of not being able to lift a cup of tea or brush your hair can be alarming. Fortunately, by understanding the causes of frozen shoulder and implementing targeted prevention strategies—including the support of an experienced osteopath—you can significantly reduce your risk and maintain optimal shoulder health.
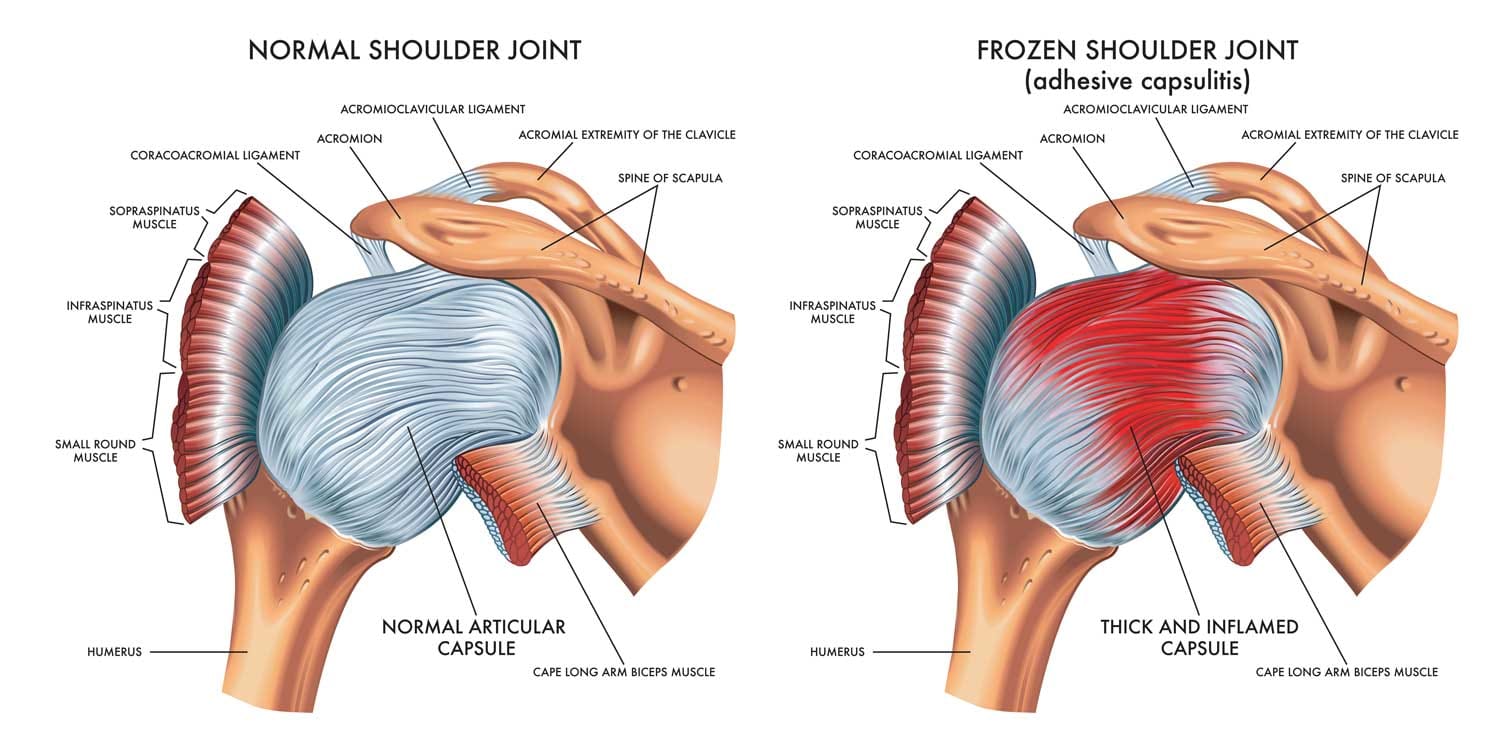
Frozen shoulder affects the shoulder joint capsule, causing it to stiffen and tighten. As a result, the shoulder becomes painful, and its range of motion diminishes considerably. Although the exact pathological processes remain under investigation, adhesive capsulitis generally progresses through three stages:
During each phase, everyday activities—such as dressing, driving or reaching for objects—can become increasingly challenging. As a result, seeking early advice from an osteopath can help manage symptoms and prevent long-term stiffness.
Frozen shoulder can arise from various medical and physiological factors. Below are some of the most significant contributors:
People with diabetes are up to five times more likely to develop frozen shoulder than the general population. High blood sugar levels can lead to changes in connective tissue collagen, causing the joint capsule to thicken and lose elasticity.
After shoulder or chest surgery—such as rotator cuff repair, mastectomy or cardiac procedures—prolonged immobilisation can precipitate adhesive capsulitis. Without regular gentle movement, the capsule can contract around the joint, leading to pain and stiffness.
Significant trauma to the shoulder, including fractures, dislocations or soft-tissue tears, can trigger inflammatory responses. Subsequently, scar tissue formation within the joint capsule may limit movement and contribute to adhesive changes.
Both hyperthyroidism and hypothyroidism have been associated with an increased risk of frozen shoulder. Hormonal imbalances can affect collagen metabolism and joint health, making the shoulder capsule more susceptible to adhesive changes.
Some studies suggest a link between cardiovascular conditions—such as heart disease or stroke—and frozen shoulder. Although the exact mechanism remains unclear, reduced physical activity and vascular changes may play a role.
Beyond strictly medical triggers, certain lifestyle factors can raise your risk of developing frozen shoulder. It is therefore crucial to address these proactively:
By recognising these risk factors early, you can work with an osteopath to design an exercise and lifestyle programme that targets mobility, posture, and overall health.
Osteopathy takes a holistic approach to musculoskeletal health, focusing on manual therapy, exercise and lifestyle advice. According to the ASA’s guidance on osteopathic marketing, practitioners may legitimately claim to relieve musculoskeletal pain and improve joint mobility, provided evidence supports these claims.
Furthermore, osteopaths are regulated by the General Osteopathic Council (GOsC) and adhere to strict advertising codes, ensuring any claims are evidence-based and medically responsible, as per the.
Preventing frozen shoulder often involves a combination of medical vigilance and proactive self-care. Below are practical strategies you can integrate into your daily routine:
Firstly, ensure you perform gentle shoulder circles, pendulum swings, and wall climbs several times a day, especially if you have an existing injury or are diabetic.
Moreover, exercises such as doorway stretches, cross-body adductors and resisted external rotations help preserve capsule viscoelasticity.
In addition, adjust your chair, keyboard and monitor height to keep your shoulders relaxed. Use lumbar support and take micro-breaks every 30 minutes to stretch.
Therefore, if you have diabetes, work with your GP and an osteopath to maintain optimal blood glucose levels. Regular check-ups can mitigate collagen changes that predispose the shoulder capsule to stiffness.
After surgery, follow your surgeon’s rehabilitation protocols. However, even modest movement in the pain-free range can prevent capsular adhesion, so discuss gentle mobilisation techniques with your osteopath.
Furthermore, quitting smoking, achieving a healthy body mass index (BMI) and reducing systemic inflammation through diet—for example, by increasing omega-3 fatty acids—can all contribute to joint health.
By implementing these prevention strategies, you not only reduce your immediate risk of frozen shoulder but also support overall musculoskeletal wellbeing.

If you experience any of the following, it’s advisable to book a consultation with a qualified osteopath:
At MHV Clinic, our osteopaths are experienced in diagnosing and supporting patients through all stages of frozen shoulder. We work collaboratively with your GP or consultant to ensure comprehensive care that adheres to ASA guidance and GOsC regulations.
In summary, the causes of frozen shoulder span medical, surgical and lifestyle-related factors. However, by understanding these triggers and engaging in proactive prevention—especially under the guidance of a registered osteopath—you can significantly reduce your risk of adhesive capsulitis. Remember:
Ultimately, maintaining shoulder mobility wasn’t just about freedom of movement—it’s about preserving quality of life. If you’re concerned about shoulder pain, stiffness or are at high risk, don’t delay: book a consultation with one of our expert osteopaths at MHV Clinic today and take the first step toward a pain-free, active future.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional for diagnosis and treatment advice.