Discover how to distinguish TMJ from a toothache. Learn symptoms, treatment options, and when to see an osteopath, chiropractor, dentist, or osteopath. Early assessment is recommended.

Millions of people experience facial pain each year, yet distinguishing between temporomandibular joint (TMJ) disorders and a simple toothache can be challenging. As a result, many delay seeking the proper treatment, whether that be physiotherapy, chiropractic care, dental intervention, or osteopathy, only to see their symptoms worsen. Fortunately, by recognising key differences and red flags, you can take proactive steps to get the relief you need quickly.
In this article, we will explore:
Moreover, we’ve aligned our guidance with the Advertising Standards Authority (ASA) recommendations on health and osteopathy (www.asa.org.uk/advice-online/health-osteopathy.html). Consequently, you can trust that all advice herein is evidence-based, transparent, and free from exaggerated claims.
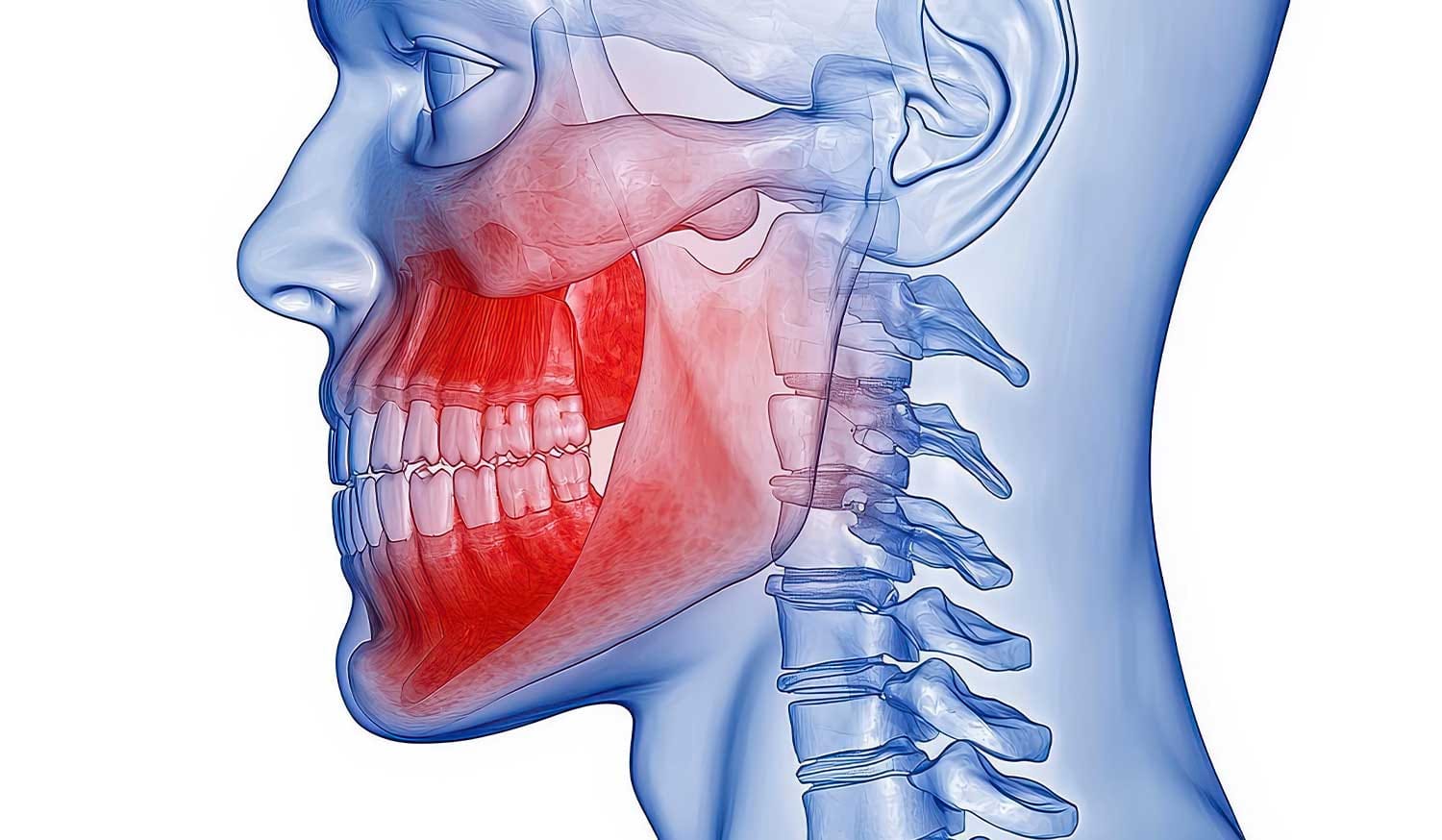
The temporomandibular joint (TMJ) acts as a sliding hinge that connects your jawbone to your skull. Because this joint is used every time you talk, chew, yawn, or swallow, any dysfunction can be particularly debilitating. TMJ disorders—often referred to simply as “TMJ”—are a collection of conditions that affect the jaw joint and surrounding muscles. Commonly, these involve:
According to the NHS (www.nhs.uk), the exact cause of TMJ disorders is often multifactorial. However, stress, bruxism (teeth grinding or clenching), injury (such as a blow to the jaw), or poor posture can predispose someone to develop TMJ symptoms.
Typically, TMJ or toothache can present with overlapping signs, making it tricky to determine the root cause. Nevertheless, TMJ disorders often manifest as:
It’s important to note that TMJ pain is often bilateral (both sides), although it can also be unilateral (one side). Meanwhile, a classic toothache typically originates from a single tooth or region of the mouth.
A toothache generally refers to pain in or around a tooth, often resulting from:
According to the British Dental Association (www.bda.org), anyone experiencing persistent, throbbing pain in a specific tooth should consult a dentist promptly to prevent complications, such as the spread of infection.
Whereas TMJ pain often presents more diffusely across the jaw and facial muscles, toothache symptoms are usually more localised. These include:
If you press on a painful tooth and feel a “pocket” or noticeable swelling, that could indicate an abscess. In such cases, visiting a dentist without delay is crucial to prevent the systemic spread of the infection (www.nhs.uk).
When facing jaw or facial pain, the fundamental question becomes: Is this TMJ or toothache? Below is a comparative overview to help decipher the two.

By carefully evaluating these factors, you can better discern whether you are dealing with TMJ or a toothache. However, it’s always best to seek professional assessment—especially if symptoms persist beyond a few days or worsen.
If any of the following apply, schedule a dentist appointment promptly:
In such cases, delaying treatment could lead to systemic infection, potentially requiring antibiotics or even hospitalisation (NHS, www.nhs.uk/conditions/tooth-abscess).
You’re likely dealing with TMJ if you notice:
Once you suspect TMJ, consider booking an early assessment with a physiotherapist or chiropractor. Both professionals are trained to evaluate musculoskeletal conditions, including temporomandibular joint (TMJ) dysfunction. Moreover, qualified osteopaths can also assess and manage TMJ disorders through gentle manipulative techniques, always ensuring adherence to ASA guidelines for non-misleading health claims (www.asa.org.uk/advice-online/health-osteopathy.html).
Physiotherapy can play a vital role in alleviating TMJ symptoms by:
According to Chartered Society of Physiotherapy guidance (www.csp.org.uk), early physio intervention often prevents TMJ issues from becoming chronic, thus reducing the need for more invasive treatments.
Chiropractors focus on aligning the spine but are also trained to treat TMJ dysfunction via:
For best outcomes, ensure your chiropractor is registered with the General Chiropractic Council (GCC) and follows evidence-based protocols. You can verify qualifications at www.gcc-uk.org.
Osteopaths often use manual and cranial techniques to manage TMJ disorders. However, in line with ASA guidance, any claims about the efficacy of such treatments must be accompanied by clear, verifiable evidence and disclaimers, such as: “Individual results may vary, and osteopathic care should complement—not replace—medical or dental advice.” For more information about compliant advertising, visit www.asa.org.uk/advice-online/health-osteopathy.html.

Below is a practical checklist to help you self-assess before reaching out to a professional:
If most signs point towards TMJ, it’s sensible to consult a physio, chiropractor, or osteopath for assessment. Conversely, if signs indicate a dental cause, book an appointment with a dentist without delay.
A dentist will typically:
If an abscess is detected, treatment typically includes root canal therapy, extraction, incision and drainage, and the administration of appropriate antibiotics. For cracked teeth, a crown or onlay may be recommended.
Physiotherapists, chiropractors, and osteopaths use a musculoskeletal approach:
Following assessment, practitioners may classify TMJ dysfunction as:
Based on the findings, they’ll devise a tailored plan that may include manual therapy, exercise, education, and referrals if necessary.
Minor Decay or Sensitivity:
Advanced Decay or Infection:
Cracked Tooth:
After definitive treatment, your dentist may discuss preventive strategies such as improved oral hygiene, diet modification to reduce sugar intake, and regular check-ups (www.bda.org).
TMJ treatment often involves a multi-disciplinary team comprising physiotherapists, chiropractors, osteopaths, dentists (especially if occlusal splints are indicated), and, in some cases, psychologists (for stress management).
Always discuss the evidence base and realistic expectations; in line with ASA guidance, osteopathic practitioners should avoid overstating benefits and instead provide balanced information (www.asa.org.uk/advice-online/health-osteopathy.html).
Where bruxism is a contributing factor, dentists may prescribe a stabilisation splint (commonly called a night guard). This removable appliance helps:
Notably, occlusal splints should be customised by a registered dental professional to ensure proper fit and avoid exacerbating symptoms.
Always follow dosage instructions and consult your doctor if you have any contraindications (e.g., gastrointestinal issues, kidney disease).
Whether you suspect TMJ or toothache, early assessment dramatically improves outcomes:
According to NICE guidance (www.nice.org.uk), early intervention for musculoskeletal disorders typically reduces pain, increases function, and lowers overall healthcare utilisation.
When deciding between a physiotherapist, chiropractor, osteopath, or dentist, consider the following:
“I first thought my pain was a toothache—sharp when biting—but my dentist found no decay. Instead, my jaw was clicking constantly. I then saw a physiotherapist who taught me exercises and gave me hands-on treatment. Within weeks, my pain reduced by 80%, and I no longer had to avoid certain foods.” – Emma, London.
“After a bike fall, I had persistent earache and jaw stiffness. My dentist ruled out a dental cause and referred me to a chiropractor. They performed gentle neck adjustments and jaw mobilisation. Now, six months later, I manage stress better and still do my jaw stretches daily.” – David, Manchester.
These real-life experiences underscore the importance of obtaining the correct diagnosis and treatment—whether dental or musculoskeletal.
Fact: While toothache is a common source of jaw discomfort, many cases are musculoskeletal (TMJ). Always consider both possibilities.
Fact: Conservative management—such as physiotherapy, chiropractic, and osteopathy—often provides more sustainable relief than medication alone.
Fact: Clicking isn’t inherently dangerous. With proper assessment and targeted exercise, many people stabilise their TMJ and eliminate clicking entirely.
Fact: Gentle, guided exercises typically help restore normal function. Avoiding any movement can lead to stiffness and worsening of symptoms.
Fact: Although there is overlap—both are non-invasive and hands-on—their core philosophies differ. Physiotherapists focus on exercise, education, and rehabilitation, whereas chiropractors emphasise spinal alignment and adjustments. Collaboratively, both can be beneficial for TMJ.
Increasingly, clinics offer both physio and chiropractic services under one roof. Such collaboration allows for:
Week 1–2:
Week 3–4:
Week 5–6:
By week six, most patients experience significant improvement in pain and function.
The Advertising Standards Authority (ASA) provides clear directives about health-related claims. To ensure full compliance:
By adhering to these principles, you ensure your communication remains ethical, accurate, and compliant with UK regulations (www.asa.org.uk/advice-online/health-osteopathy.html).
In summary, distinguishing TMJ or toothache can be confusing but is vitally essential for timely and appropriate care. While a toothache typically centres around a specific tooth—often requiring dental intervention—TMJ disorders present more diffusely, involving muscles and joints and even contributing to headaches and neck pain.
Key takeaways include:
Ultimately, whether you visit a dentist, physiotherapist, chiropractor, or osteopath, the priority is to accurately identify the cause of your pain and initiate the most effective course of action promptly. We encourage you to act at the first sign of persistent jaw or tooth pain. Early intervention not only hastens recovery but also protects your long-term oral and musculoskeletal health.
If you’re still unsure whether it’s TMJ or a toothache, don’t hesitate to contact our clinic to schedule an assessment with one of our experienced physiotherapists or chiropractors. We’ll help you pinpoint the cause and recommend a tailored treatment plan—helping you return to pain-free living as soon as possible.
References & Further Reading (UK Domains):