Discover what pelvic girdle pain is, its causes, symptoms, and effective treatments. Learn how our qualified osteopath at MHV Clinic can help you find relief.
Pelvic girdle pain (PGP) is a common yet often misunderstood condition that affects the joints and ligaments of the pelvis, resulting in discomfort, instability, and reduced mobility. Whether you’re pregnant, an athlete, or simply going about your daily routine, understanding pelvic girdle pain and how to manage it effectively is crucial. In this comprehensive guide, we’ll explore the anatomy of the pelvic girdle, delve into the causes and risk factors, highlight key symptoms, and outline evidence-based treatment options, including care from a qualified Osteopath at MHV Clinic.
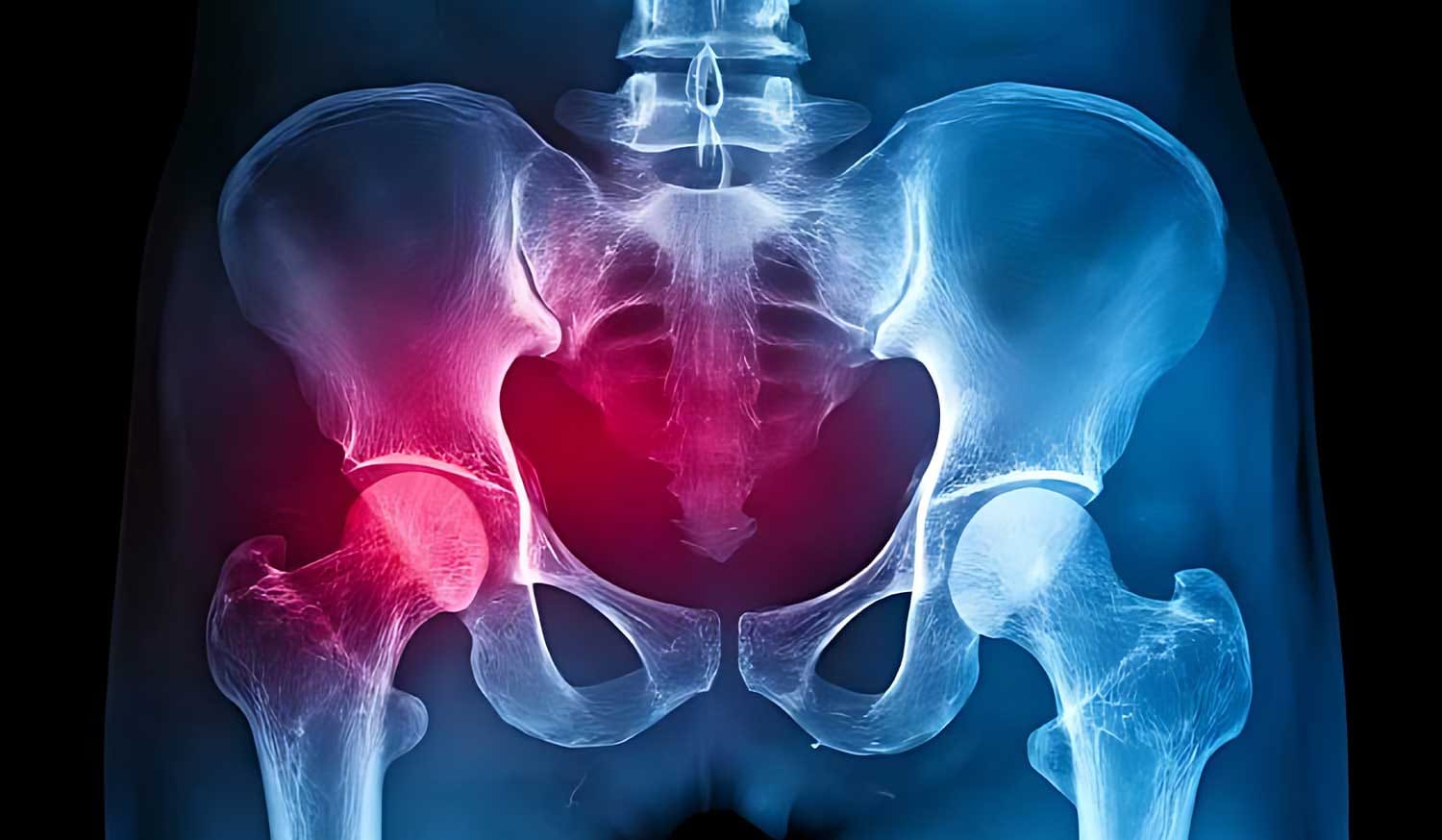
The pelvic girdle comprises two hip bones (ilium, sacrum, and coccyx), joined by strong ligaments and cartilage. This bony ring plays a pivotal role in:
However, when these ligaments become strained or joints misalign, the result can be painful, and that’s when pelvic girdle pain arises.
In simple terms, pelvic girdle pain refers to pain experienced at the front (pubic symphysis) or back (sacroiliac joints) of the pelvis. Importantly, it:
Pelvic girdle pain can be acute (short-lived) or chronic (lasting more than three months), and it often worsens with activities such as walking, climbing stairs, or turning in bed at home.
PGP can affect anyone, but is especially prevalent among certain groups:
Additional risk factors include obesity, a history of joint hypermobility and uneven leg length.

Knowing the tell-tale signs of PGP helps you seek help early. Typical symptoms include:
If left unmanaged, these symptoms can significantly impair daily activities and quality of life.
A thorough diagnosis often involves:
Early assessment by qualified professionals ensures a clear treatment plan and prevents chronicity.
Managing pelvic girdle pain usually involves a combination of conservative therapies. Below are the main approaches supported by UK guidelines:
Physiotherapists guide you through targeted exercises to:
Moreover, NICE guidelines recommend supervised exercise programmes as first-line treatment for PGP Home.
A Chiropractor uses manual adjustment techniques to:
The General Chiropractic Council regulates chiropractic care, focusing on musculoskeletal health, to ensure safe and targeted interventions.
Osteopaths registered with the General Osteopathic Council adopt a holistic approach, including:
Under ASA guidance, osteopaths may claim to treat musculoskeletal conditions, such as PGP, backing their practice with robust evidence.
Support belts can:
Taping by a trained practitioner may offer additional proprioceptive support.
Additionally, you can:
While mild PGP may improve with self-management, consult a healthcare professional if you experience:
Early intervention by an Osteopath or Chiropractor can prevent progression and restore function more rapidly.
To minimise your risk of recurrent pelvic girdle pain:
Through proactive measures, you can maintain a stable and pain-free pelvis.

Q1: Is pelvic girdle pain the same as pelvic floor dysfunction?
Not quite. While PGP originates from the joints and ligaments, pelvic floor dysfunction involves the muscles that support pelvic organs. However, both can coexist and benefit from similar rehabilitation exercises.
Q2: Can men get pelvic girdle pain?
Yes. Although common in pregnancy, men and non-pregnant women can develop PGP due to injury, poor posture or muscle imbalances.
Q3: How long does pelvic girdle pain last?
With proper care, acute PGP often improves within 6–12 weeks. Chronic cases may require longer, but consistent therapy yields positive outcomes.
Q4: Is surgery ever needed?
Surgery is extremely rare and typically reserved for severe, structural issues not responsive to conservative treatment.
Pelvic girdle pain can significantly impact your quality of life, but it is identifiable and treatable. By understanding pelvic girdle pain, recognising its symptoms, and pursuing evidence-based care — whether through exercise therapy, a qualified Chiropractor or an experienced Osteopath — you can regain stability, reduce discomfort and return to full activity.
If you’re struggling with pelvic girdle pain, don’t hesitate to contact MHV Clinic. Our multidisciplinary team of registered Osteopaths will create a bespoke treatment plan, ensuring safe and effective relief, as well as long-term pelvic health.
References & Further Reading
By integrating professional insights from our Osteopath specialists, MHV Clinic delivers comprehensive pelvic girdle pain care, empowering you to move confidently once more.